It’s been too long since I updated on our off-road journey across unknown territories.
To briefly recap, in early 2013 we jumped off a cliff and hoped for a soft landing.
We removed all barriers obstructing instant access to a GP, and removed the dam which was holding back the floodwaters. What happened next (over 2013 and 2014) is well documented in previous blogs, and it hasn’t always been an easy cruise.
But we’ve changed.
We’ve learnt. We’ve moulded. We’ve morphed.
And I think we’re all the better for it.
To get us started and for the first year, we closely followed a strategy developed by a company called Doctor-First (meaning the patient gets to speak to the doctor first, not that the doctors are put first as many like to suggest!). The ethos is simple: the most senior person (namely the GP) speaks to the patient first, identifies their needs, and directs them in the most appropriate way in order to minimise delays in their care and maximise efficiency. This avoids wasting patients’ and NHS time by giving them inappropriate appointments with the wrong person.
In an ideal scenario, the receptionist would be bypassed altogether and the incoming phones lines would all be directed straight to the desk tops of an army of GPs who would be waiting to deal with them. We didn’t get away with this. Data over the years has shown the patient demand in our Practice to be higher than the local (and National) average and despite 5 incoming phone lines and 5 GPs at the ready, there was no way we could keep up and stem the flow of calls between 8 and 9am. So from early on, we found need to adapt from the purist form of this model. The receptionists took the calls as usual and added them to the GP callback list of the patient’s choice.
For the first 6-12 months the improved satisfaction from patients (who were all too familiar will being ‘turned away’ through lack of appointments in the previous system) was palpable. Complaints hit an all time low. Everyone was happy.
Before long though, the frustrations started to creep in. There is no doubt that to some extent this was due to a raising of the bar in terms of expectations. Patients could now be guaranteed to see a GP on the same they rang – regardless of urgency – but they did have to wait anywhere between 5 minutes and 4 hrs for a callback to agree an appointment time, or to get advice. (The wait time was determined by the GP who prioritised the perceived urgency of the callback based on the information provided by the patient to the receptionist).
By the start of the second year, problems started to arise.
We remained a whole-time equivalent GP down and had a few comings and goings within the team (GPs, receptionist and nurse practitioners) making it difficult to keep up with the training required to make the system work. Being reduced in GP numbers, the volume of call-backs per GP was higher than safe – and totally unmanageable at times of further workforce reduction such as during GP annual leave. On occasions, the daily callback list for an individual GP would reach over 120 patients. At the same time we all recognised our personal fatigue, which kicked in at around 45 patients. Cutting corners, the inability to listen, and risk of burnout became real fears.
GPs were becoming exhausted and the complaints started trickling in again.
The main issues were two-fold – ‘Why can’t I just book an appointment?’ ‘Why do I need to speak to a GP first’ ‘Why do I have to wait 4 hrs for a callback?’
So we listened. And we adapted.
By now, patients were well aware that ‘telephone advice’ was very much an option for their convenience should they prefer it. It was also clear that they were becoming quite good at knowing when they needed advice, and when they needed an examination.
They were acquiring skills that the previous traditional appointment system had not allowed or required them to develop.
2015 was a good year for us.
In August, we were fortunate to recruit a fantastic, newly trained, full-time GP. She’s a rock. Not only does she buy-in to the whole partnership/collegiality/ vocational career kind of stuff, but she’s an excellent clinician with a head on her mature beyond her years. Such recruits are hard to come by in General Practice. A few months later, our lucky streak continued when we successfully recruited and appointed not one, not two but THREE amazing Nurse Practitioners. All highly skilled with many years of experience in a variety of fields (including ITU, community matron experience and orthopaedics/MSK to name a few), this tremendous trio seem to have no end to their enthusiasm and dedication, wanting to develop specialist skills and partake in home visits.
Combined with listening to the changing needs of our patients, this new workforce gave us opportunity to make a couple of simultaneous changes.
Firstly, recognising that a new GP needs support and time to get to know their patients (and vice versa) we agreed to establish a two-tier choice system for our patients. This GP, and one other (by choice) would operate a traditional (10 minute) appointment system, as would the Nurse Practitioners (15 minutes). The remaining 3 GPs would continue to offer a telephone advice service – booking patients in for a face-to-face when appropriate, or directing them on to alternative or self-care pathways. Now, on phoning in, the patients would have the choice of booking directly into a traditional (10 minute) appointment slot with one of two GPs or a (15 minute) Nurse Practitioner slot. Or…they could choose to go on a callback list of one of 3 other GPs. This system allows patients to choose a style and/or clinician who suits their personal preference and still allows for continuity.
Secondly, the workload and GP fatigue needed addressing. The data we had collated over the previous years gave us accurate figures for our daily/weekly demand for appointments. It was clear, than when all GPs were in, 36 callback appointments for each of the triage GPs (plus the traditional appointments of the others) was more than enough to satisfy our demand and leave some spare capacity in the system. The only time demand rose above this was during periods of annual leave – and became unsafe. We calculated an ‘average’ daily figure per GP based on the information we had, added a little for extra capacity and a bit more (3% ) for year on year increase, and came up with a magic figure of ’44’.
With this hybrid system in place, the callback list for each GP rarely reaches 44 – we usually have appointments to spare – but early in the day we have the comfort of knowing that we’re protected from going beyond our safety margins. The day ahead doesn’t appear so daunting anymore. Patients are dealt with more swiftly and efficiently by a GP who is still fresh and capable. It’s not perfect – will it ever be in the current climate of underfunding? – but it’s certainly the best we’ve ever been able to offer. Yes, at times of reduced manpower, a small handful of patients are still asked to call back another day if the problem isn’t urgent, but urgent problems are aways squeezed in with little detriment to the GP. We are also fortunate locally, to be supported by an out-of-hours GP pilot which fires up after 6.30pm (see NHS Star). This is a system of local GPs working together to improve access outside core hours. However, despite governments protestations that the public want this kind of routine access, it has found itself under-utilised and is therefore allowing the appointments to be used as a kind of ‘over-flow’ service, for GPs to book into during the course of the afternoon if they are experiencing above normal demand levels.
I can count of on one hand the times we have used this a an over-flow facility over the last 6 months, but it’s nice to know it’s there. The deadline stress has been removed.
The GPs doing the ‘callback’ system feel rejuvenated and are enjoying work once more. We are acting in a true ‘GP Consultant’ role – or in other words, ‘Consultants in General Medical Care’. We advise, direct and educate 60-70% of our patients. Self-limiting conditions are managed by advice. Acute simple problems are seen by the Nurse Practitioners. This leaves longer appointment times for the GPs to see the more needy 30-40% of patients with complex conditions, mental health issues, or red flags. It’s not unusual for most of the patients I see face-to-face to have between 30 and 45mins with me. During which time they may pop in to see the nurse for essential tests and come back to me to discuss the results, or sit next to me while I speak to a local specialist for advice, or to arrange an urgent assessment.
They leave happy having had a complete one-stop service.
I go to bed knowing I haven’t cut corners.
Sad as I am to admit it, this is in stark contrast to much wasted time we have in the NHS.
A few weeks ago I spoke to an elderly patient who proudly advised me that she’d called the paramedics out at 2am that morning for a ‘sweat rash’ on her chest which was interfering with her sleep. The paramedics referred her on to NHS111, who, after a lengthy phone assessment, sent out a visiting nurse to check her. The nurse attended at 5am, confirmed the diagnosis, and advised her to call her GP in the morning to request an appointment to get some cream. Between 2am and 8am, this patient had had 4 contacts with the NHS, and 5hrs of NHS time. This, for a condition which would have been sorted in a two minute GP consultation.
How have we ever allowed this to happen?
That same day, another lady had suffered with foot pain all day, and decided at 8pm she’d really like to see a GP. She followed the practice procedure for an out-of-hours appointment and called NHS111 in the hope of accessing an evening GP appointment, to which her daughter would gladly transport her. Again, after a lengthy NHS111 phone assessment, the advisor on the phone determined that it was ‘not safe’ for her to travel to an appointment, but required a blue-light, 999, ambulance. The lady – who felt otherwise well- and her daughter, protested vehemently to this suggestion, but to no avail. By now it was almost 9.30pm. The paramedics arrived promptly and were ‘delightful and thorough’ and sensibly realised very quickly that this was not a blue-light situation. By 11pm the paramedic assessment, together with paperwork, was complete. The lady was reassured, and advised to see her own GP in the morning for a reassessment.
By next morning, her pain had gone.
This kind of onerous, labour intensive practice is commonplace in the NHS. At the same, all over the UK, GP practices are closing because the funding doesn’t match the demands. Local doctors have no spare capacity to take on their patients. As demands and expectations continue to rise, so does stress and burnout amongst clinicians, with no new doctors coming along to replace them.
As patient numbers are rising, so are GP vacancies.
Any individual GP practice can’t supply a system that suits ALL patients. In order to maintain our sanity, we first need to accept this. Doctors tend to be individuals who have spent their life trying to please everyone – their parents, their teachers, and now their patients. They don’t like to provide a less than perfect answer.
Patients and GPs need to make a choice. Just as they might choose which GP to see within a practice for differing skill sets and personalities – they should also be able to choose (or leave!) a practice with an extensive telephone appointment system.
Not all our patients are happy. They never will. But this is by far the most popular and least complained about system we’ve ever operated. And importantly, the GPs feel it’s sustainable.
Work has never felt happier.
Who knows, we may even make it to retirement.
The system which Doctor-First preaches, is not rocket science. Anyone can have a go, but we have them to thank for giving us the support and confidence to embark on this journey. We’ve been very fortunate with our superb clinical team and very patient patients (!) but the real heroes here are the reception staff. They have really turned things around. Discreetly and tactfully, they seek just the right amount of information from each patient, to enable the GP to priorities the call in terms of urgency, but also to help guide and advise the patient who might be the most appropriate clinician for the their needs. Our skilled reception staff also have a good idea who and what might need a ‘hands-on’ face to face appointment, and which potentially self-limiting problems might be better encouraged to have an advice appointment first. Without them on-board, this system would be a certain failure. Good reception training and support is essential to this system.
It’s been a challenging journey with ever changing topography. The initial path was cobbled and previously unchartered. Next we stumbled through mountainous landscape with steep inclines and rapid descents. The terrain will continue to change depending on what is thrown in our path in an attempt to block our progress – but one thing is for sure, we have no desire to retrace our steps and go back.
Who knows what the road ahead will look like, but at the moment we’re just pausing to enjoy the view – and the journey has been worth it. 🙂

***
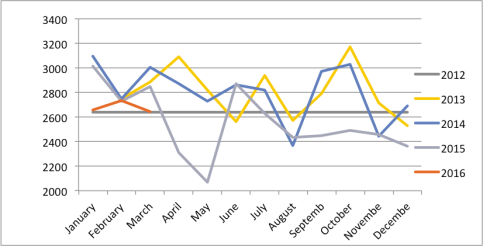
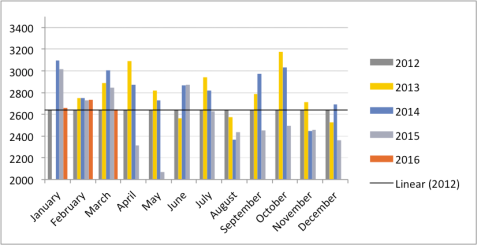
Images showing demand data (= patient contacts)
2012 (Pre-change). Traditional system – flat rate appts/month
2013 First year ‘Doctor First’ system
2014 Second year ‘Doctor first’ system
2015 August – development of hybrid two-tier system
2016 Ongoing
We had feared year on year increased demand, but this has not been noted. But we are now comfortably offering far more patient contacts than we did with the traditional linear system.

An obvious solution to the problem….called compromise…why did it take so long to introduce, after all that’s what the patient feedback was saying.
I think you all do an amazing job you all seem more relaxed as a pt with complex problems I usually speak to my named GP as I think continuity is important your all stars ☺xx
Thanks Gerry. Nice to hear. I for one, certainly feels more relaxed. Glad others come across likewise. Much less stressed all round I think – this can only be beneficial for patients.
And thanks for your ongoing support with shaping the practice.
Pingback: Round up: GP wellbeing, compassionate leadership & listening to patients – Good doctors
This is good it is what patients would like when needing appointments this will improve patient feedback
Well done Dr Wethetell that is the exact tack I was trying so hard to steer you down in 2013 and as you say it is not rocket science. Resistance to change never wins in the end. Junior Doctors take note.
Thanks George. I’m sorry I don’t recall that steer in 2013 but I also don’t think it was the right time. To introduce a two-tier system from the outset would have been very confusing for many patients – not knowing what or how to choose, and not being familiar with the concept of telephone appointments. I think the system has evolved at a sensible pace, and patients – now well versed in the option of telephone consultations – seem well placed to make the most appropriate choice.
Hope you don’t feel we are resistant to change! I don’t know of many practices who are comfortable to take on as many changes as we have in such a short space of time.
Got there in the end at least! 🙂
Heather. …the National survey was telling that you needed to change the process that was the whole purpose of me putting together a patient survey. You would have had the feedback to work with earlier.
Never underestimate customer feedback it is a powerful tool.
Gathering email addresses earlie again would have given you a positive and continuous line of communication. Overall the feedback and communication channel through email would have taken the stress away by given you early warnings that things were not as they should be. Therefore reducing staff turnover and stress.
You now need the patients to tell you that you have got it right through positive feedback from the National Survey.
Having said all of that well done.
Totally agree re feedback – it’s our most powerful tool, but I’m still not sure we could have acted on feedback before we’d changed the system in 2013! (This change was of course also a result of feedback).
Thanks again for your help. Like you say – fingers crossed for the next survey!