Let’s hope it’s not a train…!
“Definition of insanity – Doing the same thing over and over again and expecting different results”
Albert Einstein.
It’s been a deliberately long time since my last update. I wanted to report some news.
Things have been ticking along quite nicely. On some days, I’ve even thought …This is it…. we’ve cracked it
Not bad considering we’ve spent the last 12 months trying unsuccessfully to recruit another GP (along with the rest of the Nation) and are still working with far fewer GP sessions (and far greater patient list sizes) than we’d really like.
For those new to this blog at end of January 2014, we be celebrated the first anniversary of our new appointment system – where the most senior clinicians take all the calls, and together with the patient, determine the best course of action. GP appointments are no longer booked by the receptionist at the request of the patient, leaving ample appointment availability for those who need them most. (see earlier posts for the background and implementation of this system).
16 months on, and we’re surviving, but the past year has indeed seen some tough challenges.
We welcomed a new GP Partner in January 2013. She left 6 months later.
We welcomed a New Nurse Practitioner in August 2013. She lasted 3 months.
Finally, a 7 session GP partner handed in his resignation in October 2013 and went on long-term sick leave a month later. We ended 2013, 14 clinical sessions per week down. 😦
It would be unfair to say that this was any reflection on the new appointment system. The bitter truth is, we’d lost a similar number of key players over recent past years, even with our traditional appointment system. 21st Century NHS General Practice is tough. Expectations and demands on us are high, from all those who have a vested interest in our services – whether they be patients, politicians, secondary care services, solicitors, insurance companies, employers or the media. They each demand a ‘piece’ of our time and expertise, and all have their own agenda and needs.
Things picked up in February 2014 when we were lucky enough to recruit and welcome, a fantastic replacement for our first out-going GP partner of the previous year. We are currently (and at last!) in the interview stages of replacing our second outgoing Partner, and there is a BIG beam of light shining at the end of our tunnel…..(maybe even TWO BIG beams of light….)
So how about the telephone appointment system? Are we still surviving? And how about our patients?
Firstly, I’d like to dispel a few common myths and commonly expressed concerns.
1. The system discriminates against deaf patients or those who are unable to use the telephone.
We have a handful of deaf patients, some of whom rely on sign language or lip-reading, but we have many more who are simply elderly with impaired hearing and find the telephone difficult for any more than a brief conversation.
Our appointment system shouldn’t pose a problem to them at all.
What needs to be emphasised is that this system is a not a replacement for seeing the doctor in a traditional face-to-face appointment. It’s simply an alternative option for those who want telephone advice for their own convenience.
We already know about many of our hard-of-hearing patients, and their notes are marked a such; others we asked to alert us to this problem. These patients can just as easily book a face-to-face appointment with their chosen GP as they as they did in the old system – In fact more easily so, as we actually have free appointments available for them every day – all day – unlike the old system when all appointments were taken by 8.10am!
2. The ready availability of GP access over-nurtures our patients, raises their expectations and increases year-on-year demand
One thing that has really surprised me (and appealed) about this way of working, is how much easier it is to encourage self-care or appropriate watchful-waiting over the telephone than it is with the patient sitting next you already with the expectation of a prescription – or some other convenient form of management. Patient education is important and ongoing, with ‘information printouts’ being left to collect, or ‘web-links’ being shared, at least as frequently as prescriptions. What is also refreshing to see, is just how welcoming patients are to this approach of healthcare.
After completion of our first 12 months, we have been able to start collecting accurate month-by-month comparison data on demand, and will continuing collecting such data year on year. Prior to February 2013 (like most traditional practices) we could only ‘estimate’ demand by how many patients actually managed to get the appointments which were on offer. We now know exactly what our daily demand is, to the dot.
Our “demand” is defined as anyone who needs a GP to make a clinical decision for them. This may be to see and examine them; to consider and advise on their symptoms; to request for a medication which has not been authorised as a regular repeat for them; to request a sick note, or a letter; or sharing of a blood result or hospital communication. This is true demand of a GPs workload in today’s NHS.
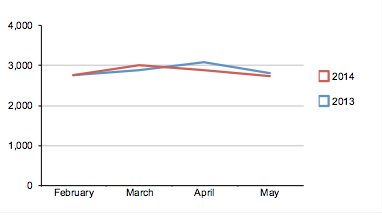
We have only 4 comparison figures so far (Total patient-GP contacts for months of February, March, April and May) but the graph below shows our 2014 demand (red) compared to 2013 (blue).
The a slight fluctuations in April and May tallies with in which month the Easter and Spring bank holidays fell each year. Apart from that, demand has been pretty static so far. Given that most GPs would expect to see a slight year on year rise in demand Nationally, maybe this plateau is even more significant than it first appears?
Fingers crossed. Only time will tell.
3. OK – but telephone consulting is just ‘bad news’ this is not what ‘being a good GP’ is about….
It is true, we gain a lot of ‘soft knowledge’ from our patients and their families when seeing them face-to-face and one GP recently commented on Dr Jonathan Tomlinson’s “A Better NHS” blog, that a telephone based consultation risks missing those “critical door-handle moments”. The beauty of the system we use is that by allowing much greater use of, and access to, telephone consultations by those who actively ‘want’ them (in our experience around 60-70%) then we free up face-to-face consultations for the rest who really need a face-to-face appointment. Indeed, in our experience, it is this latter group (30-40%) who are more likely to be those ‘door-handle-moment’ patients.
In fact, all we have done is create a ‘distillate of need’ and freed-up more GP time for those that do really need it.
In summary, the job is immensely more satisfying. Both doctors, staff and patients are happier and more relaxed.
The patients are well versed in self-care – yet know they can see the GP (of their choice) whenever they need.
And all this whilst working at 8 GP-partner sessions down on our of capacity of 1yr ago? Yes, there have been some hard days – but is that really so surprising?
Are we nurturing a rise in our patients’ expectations? Yes, I suspect we are. In any service, the more you exceed expectations, the higher you raise the bar. Two years ago we had a steady stream of complaints from people complaining they had to wait 3 weeks to get an appointment with the doctor of their choice. Now we get complaints they have to wait up to 3hrs (on a busy day) for that same GP to phone them (to arrange a same-day appointment). Heigh-ho…
This is something we just have to manage. Complaints, however, are notably fewer.
The other thing to manage is perception of need. There is a fear, in both patients and doctors, of ‘missing something’ if a patient is not seen. This is a complex one. What of the patient with a simple presentation, who went on to have an adverse – but possibly unrelated – event 48hr later? How will we ever know if the outcome would have been any different if the GP had seen him/her? And would this situation have been easier, or harder, for the patient/family/GP to accept if a GP had seen him/her and potentially ‘missed’ something in a face-to-face consultation? There are so many ‘unknowns’ and emotive factors in this scenario. The default is always to see the patient who wants to be seen, but what if both patient and GP had willingly agreed on the management plan not to be seen?
***
Adopting this type of approach in Primary care is quite a radical change. We have done things the same old way for a long time now. But, as Dan Rockwell recently wrote – we too often believe that repeating the past will produce more success…But in a changing world, repeating the past makes us irrelevant. The danger of success is repetition. But the opportunity of failure is transformation.
Times are tough out there. Newly trained doctors are not choosing General Practice as a career, experienced GPs are retiring young and yet the workload continues to escalate. Only this week we heard the news that up to 40% of GP training posts now remain unfilled in some areas. At the same time, the Government – recognising the workforce crisis – are declaring to make General practice the ‘Career of choice’ for at least 50% of new doctors. I wonder how they are planning to achieve this?
The NHS is a cost efficient delivery means for health as demonstrated by this image shared recently through the Executive summary of the by the Commonwealth Fund which shows ranking of healthcare relative to National spend per capita:
What’s more – UK General Practice delivers 90% of these NHS contacts, on just 8.4% of the total NHS budget.
The government knows just how efficient UK General Practice is at delivering healthcare. Just imagine what we could do with even a small amount of additional funding?
Funding would help make the job more attractive, certainly – but let’s make one thing clear – when GPs ask for ‘more funding’ what they are asking for is funding to provide more doctors for their patients. That is, more GPs to allow for a better doctor-patient ratio, in turn allowing for more time per patient and a better quality of care. We’re not demanding better incomes – just more manageable and (most importantly) safer workloads.
The Royal College of General Practitioners’ “Put Patients First campaign” is campaigning for an uplift in funding of just 2.6%, to direct 11% of the NHS budget to Primary care, by 2017.
Meanwhile, the only thing we can do to make the job more attractive is take back some control. In these difficult circumstances, at least we’re trying to do our best.
What I can’t stress enough is that this system is no substitute for a strong workforce. As we have discovered, it is not a solution for an under- resourced practice who are struggling to recruit and are reluctantly working at well above the National average list size. But, if you have a full complement of experienced GPs, who work well as a team, know their patients, and who are willing to try and make a better life for themselves and for their patients, then go on…..go for it….give it a go….
Don’t let what you can’t do, stop you from doing what you can.
You know you want to. 🙂
Conflict of Interest declaration:
Owing to the success of our Practice’s implementation of this appointment system over the past 12months (and as a result of this public blog) we were approached earlier this year by Productive Primary Care’s “Doctor First” team and ask if we would be happy to become a training/mentor Practice for other GP surgeries who were embarking on this journey. So far we have mentored one such Practice, and were paid to do so by Productive Primary Care.
( No interest in persuading you to take it up though, other than I just feel it works well for us!! :))


Lovely honest blog nice to read
I am a patient, I like telephone consultations, helps me and helps the practice. I also like being a competent self-manager and being able to self-refer to neurophysiotherapy or the continence team. As for the door handle patients, I know that learning to set the agenda pts and drs helps this. I’ve seen it, I am a patient who co -runs a training consultancy. Doctors need training to support self-management and implement the house of care. Good luck